🎯 Case Highlight: Superior Vena Cava Syndrome in a Young Dialysis Patient
By Dr. Omar Hamdallah, Vascular and Endovascular Surgeon
Patient: 17‑year‑old female
Medical History: End-stage renal disease (ESRD), on maintenance hemodialysis via a tunneled dialysis catheter (Permacath) for 1 year.
🩺 Clinical Presentation
The patient presented with progressive swelling of the face, neck, and upper chest, along with difficulty breathing and visible chest wall veins. These are hallmark signs of Superior Vena Cava Syndrome (SVCS)—a condition resulting from impaired venous return to the heart due to obstruction in the SVC.
🔍 Diagnostic Workup
• Clinical suspicion was raised for central venous stenosis, a well-known complication in dialysis patients with long-term central catheters.
• Venography revealed a critical high-grade stenosis of the superior vena cava, just proximal to its junction with the right atrium.
• The dialysis catheter also exhibited poor flow, likely secondary to venous congestion and stenosis.
🛠️ Intervention – Performed by Dr. Omar Hamdallah
Given the severity of the stenosis and the patient’s symptoms, I proceeded with a minimally invasive endovascular treatment:
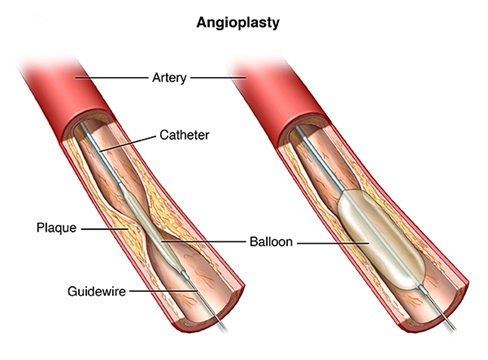
1. Vascular Access: Secured under ultrasound guidance, followed by catheter placement to perform diagnostic imaging.
2. Venography: Confirmed a >90% tight stenosis of the superior vena cava, with significant collateral formation and delayed contrast transit.
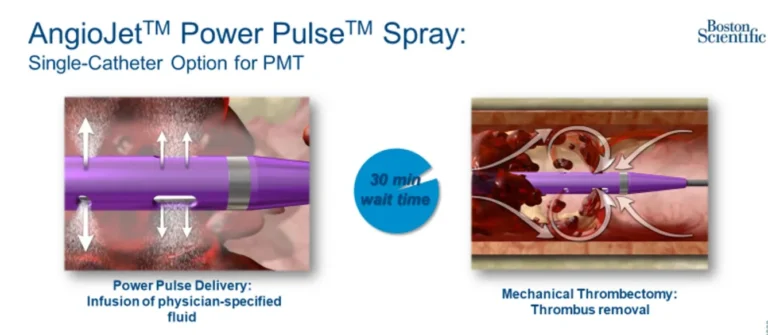
3. Balloon Angioplasty:
• Performed serial balloon dilatation using high-pressure balloons, starting with smaller diameters and progressively increasing size.
• Inflation was done gradually to minimize vessel trauma while effectively opening the narrowed segment.
4. Post-Dilatation Imaging: Revealed significant improvement in venous caliber and flow, with decompression of collaterals and normalization of contrast return.
5. Clinical Outcome:
• The patient experienced immediate relief of facial and upper body swelling.
• Respiratory symptoms subsided within hours.
• Dialysis catheter flow improved, allowing uninterrupted dialysis sessions.
• No complications occurred during or after the procedure.
This case illustrates the efficacy and safety of percutaneous balloon angioplasty in managing SVC syndrome, particularly in young dialysis patients, avoiding the morbidity of open thoracic surgery.
📘 Patient Education
What Is Superior Vena Cava Syndrome?
SVCS is caused by a blockage or severe narrowing of the superior vena cava, the large vein that drains blood from the head, neck, and upper body back to the heart. In dialysis patients, long-term catheter use can lead to scarring, fibrosis, and stenosis of central veins.
Common Symptoms:
• Facial and neck swelling (especially upon waking)
• Arm and chest swelling
• Difficulty breathing or coughing
• Prominent chest wall veins
• Headache or dizziness in severe cases
Why Are Dialysis Patients at Risk?
• Prolonged use of tunneled catheters (like Permacaths) leads to chronic vein irritation, increasing the risk of central venous stenosis.
• High blood flow through an arteriovenous fistula (AVF) can worsen pressure buildup in already narrowed veins.
🧩 Treatment Options for SVC Stenosis
Treatment Description Pros & Considerations
Balloon Angioplasty High-pressure balloon used to widen the narrowed vein Minimally invasive; first-line option; safe and effective but may require repeat procedures
Stent Placement Metallic scaffold inserted to keep the vein open Used if angioplasty is not durable; covered stents may offer better long-term patency
Surgical Bypass Open surgery to reroute blood flow Reserved for refractory cases; more invasive with higher surgical risk
HeRO Graft or Femoral Access Alternate dialysis access routes bypassing central veins Used when upper body access fails
Flow Reduction Techniques Reduces AVF flow to prevent venous hypertension Considered if high-flow AVF contributes to symptoms or recurrence
🧠 What You Should Know as a Patient
• Don’t ignore symptoms like swelling or shortness of breath—these may signal serious vascular issues.
• Avoid prolonged catheter use when possible—early planning for AV fistula creation reduces long-term risk.
• Regular follow-up is critical after any central vein intervention to monitor for recurrence.
🌐 Recommended Resources
• National Kidney Foundation – Central Venous Stenosis
• Frontiers in Nephrology – Central Vein Stenosis Review
• MedlinePlus – Superior Vena Cava Syndrome
• Wikipedia – Superior Vena Cava Syndrome
✅ Final Thoughts
This case is a strong reminder of the vascular complications that can arise in young dialysis patients. Early detection, appropriate imaging, and timely intervention can significantly improve outcomes and avoid invasive procedures.
If you or a loved one is on dialysis and experiencing similar symptoms, seek prompt evaluation. At Jordan Vascular Clinic, we specialize in minimally invasive vascular treatments to restore circulation and preserve dialysis access.
📍 For appointments and consultations with Dr. Omar Hamdallah, visit jordanvascular.com
![Dr Omar Hamdallah الدكتور عمر نادر يونس حمدالله [Dictation ended]](https://jordanvascular.com/wp-content/uploads/2025/10/cropped-Untitled-1.png)